Clear communication is a clinical safety issue. For deaf and hard of hearing (DHH) patients, misunderstandings can lead to inaccurate histories, consent problems, poor adherence, and avoidable dissatisfaction.
Communication Tips for Deaf and Hard of Hearing Patients
Mar 1, 2026 7:00:00 AM / by PICA Risk Management Specialist posted in Risk Management, Compliance
Insurance Investigations Triggered by Patient Complaints
Feb 3, 2026 5:35:28 PM / by PICA Risk Management Specialist posted in Compliance, Practice Management
Insurance investigations arising from patient complaints are increasingly common and may be your first indication that the patient had a concern about the care you provided or about your billing practices. These inquiries may originate from commercial insurers, Medicare Advantage plans, Medicaid managed care organizations, or government contractors acting on behalf of Centers for Medicare & Medicaid Services (CMS).
Regulatory Compliance Updates for 2026
Jan 9, 2026 11:36:12 AM / by PICA Risk Management Specialist posted in Compliance
As we start the new year, it is a great time to review regulatory updates and implement necessary changes to reduce your risk. This article summarizes billing and coding changes as well as HIPAA updates.
Avoiding Scope-of-Practice Violations
Nov 26, 2025 11:22:20 AM / by PICA Risk Management Specialist posted in Compliance, Practice Management
Scope-of-practice violations are among the most common – and costly – regulatory risks for doctors and medical practices. These occur when:
- A provider performs tasks they are not legally permitted or trained to do.
- Tasks are delegated to staff whose licensure does not authorize those activities.
Scale Your Practice & Maintain Quality Care
Oct 24, 2025 1:22:53 PM / by PICA Risk Management Specialist posted in Compliance, Practice Management
In today’s rapidly evolving healthcare landscape, many physicians are seeking ways to grow their practices without compromising the quality of care. Scaling a medical practice involves more than simply seeing more patients - it requires strategic expansion of operations, staffing, technology, and patient engagement systems. When done correctly, it can increase profitability, improve efficiency, and enhance patient satisfaction. Below are steps you can take to scale your practice.
Texting with Patients: The Risks and Safer Alternatives
Sep 10, 2025 5:40:00 PM / by PICA Risk Management Specialist posted in Risk Management, Compliance
Nearly everyone texts to communicate. It’s quick, easy, and convenient. However, texting with patients carries professional, legal, and ethical risks, including:
- Privacy and HIPAA compliance. Standard texting is not secure. Messages can be intercepted, viewed on shared devices, or accidentally sent to the wrong number. Therefore, any patient’s personal health information sent via text risks a HIPAA violation and possible fines.
Major Changes Proposed for Medicare Reimbursement of Skin Substitutes
Aug 5, 2025 10:59:34 AM / by J. Kevin West posted in Compliance
The Centers for Medicare & Medicaid Services (CMS) has proposed significant reforms to the Medicare Part B payment methodology for skin substitute products. If adopted, the proposed changes1 would significantly decrease the reimbursement rate for such services.
Compassionate, Inclusive, and Competent Healthcare: Focus on the LGBTQIA+ Community
Jun 6, 2025 11:40:44 AM / by PICA Risk Management Specialist posted in Compliance, Practice Management
While most healthcare providers are compassionate and want to provide optimal care to their patients, implicit biases exist. Healthcare providers may not be aware of implicit biases, which may be subtle and unintentional, that can influence clinical interactions, lead to a lack of trust between the patient and the healthcare provider, and result in healthcare disparities.
You Just Received a Negative Online Review… Now What?
Apr 11, 2025 11:41:16 AM / by PICA Risk Management Specialist posted in Compliance, Practice Management
All healthcare professionals like to receive positive online reviews. It’s a great way to let people know about you and the exceptional care you provide. Which, in turn, can help send new patients your way.
Releasing Patient Medical Records to Medicare, Medicare Advantage, and Insurance Companies
Mar 10, 2025 2:22:43 PM / by J. Kevin West posted in Compliance
A doctor’s obligations regarding how to respond to medical records requests from Medicare, Medicare Advantage, and insurance companies can easily cause confusion. Receiving medical records requests is a frequent and common occurrence and it’s important to note that responding to these records requests does not require the doctor to acquire a medical records release form from the patient first.
HIPAA Rules for Releasing Medical Records
In fact, HIPAA allows medical records to be released without a patient release form in many different settings, including for patient treatment, billing, etc. Because HIPAA allows information sharing for billing purposes, any language on a CMS 1500 form is superseded by HIPAA guidelines – the CMS 1500 form does not prevent a release of records that is otherwise allowed by HIPAA.
Regarding record requests from Medicare, Medicare Advantage, or commercial insurance plans, HIPAA also allows the doctor to provide medical records without a patient release form. HIPAA allows sharing of patient records for purposes of “health care operations,” which includes quality control, audits, licensure matters, etc. Additionally, most (if not all) provider agreements contractually require doctors to provide records to the insurer or to Medicare upon request and doing so does not require a patient release form.
Patient Medical Records Release Forms vs. Informed Consent Forms
Also keep in mind that a patient medical records release form is different from an informed consent form. A medical records release form pertains to the sharing of health information, while an informed consent form relates to the authorization of medical procedures or treatments after understanding the associated risks.
Comply with Medical Records Requests to Avoid Issues
A simple and reliable recommendation is that doctors comply with record requests from Medicare, Medicare Advantage, and commercial insurers, and remember that patient medical releases are not required to do so. Furthermore, refusing to comply with record requests is playing with fire – Medicare can revoke a doctor’s billing privileges for refusing to comply, and insurers can terminate the doctor’s provider agreement for failure to comply. It is never advisable for a provider to withhold or refuse to provide records in response to a request from a payer, whether governmental or private.
Medicare Finalizes Skin Substitute Graft Policies: Changes Coming in February
Jan 7, 2025 2:35:57 PM / by PICA Risk Management Specialist posted in Compliance
UPDATE 2/10/25: The Feb. 12, 2025 date referenced in this article has been delayed to April 13, 2025 by all seven Part B Medicare Administrative Contractors (MACs).
The Centers for Medicare & Medicaid Services (CMS) recently finalized Local Coverage Determinations (LCDs) for skin substitute grafts and Cellular and Tissue-Based Products (CTPs). Released by all seven Part B Medicare Administrative Contractors (MACs) on November 14, 2024, these policies will govern the use of skin substitute grafts for Medicare Part B beneficiaries for services rendered on or after February 12, 2025. The new policies set forth coverage requirements and limitations, including a list of covered and non-covered skin graft products, for the treatment of diabetic foot ulcers (DFUs) and venous leg ulcers (VLUs).
HIPAA Reminders for 2025: Cybersecurity & Reproductive Health Privacy
Jan 7, 2025 11:32:38 AM / by PICA Risk Management Specialist posted in Compliance
Measures to Strengthen Cybersecurity in Healthcare under HIPAA
Solo Dental Practice Hit with $70,000 Penalty for Violation of the HIPAA Right of Access Rule
Dec 4, 2024 12:55:16 PM / by Michael Brody, DPM posted in Compliance
You might be wondering what a dental practice has to do with podiatric medicine. Well, unfortunately, your podiatric medical practice could be just as vulnerable to a HIPAA violation as any other healthcare practice. This recent case illustrates the devastating repercussions of failing to comply with the HIPAA Right of Access Rules. Read below to find out how this happened.
Prescribing Opioids – Important Information for Practitioners
Apr 17, 2024 4:54:43 PM / by PICA Risk Management Specialist posted in Risk Management, Compliance
If you prescribe opioids in your practice, it is important to be familiar with current clinical practice guidelines for prescribing opioids, DEA requirements, and federal and state laws and regulations to reduce your professional and administrative liability risk. In this article we will discuss some of the guidelines, requirements, and regulations relating to prescribing opioids.
Drug Enforcement Administration (DEA) New Training Requirements
Sep 6, 2023 12:12:44 PM / by PICA Risk Management Specialist posted in Compliance
The Medication Access and Training Expansion (MATE) Act was passed by Congress as part of the Omnibus Bill of 2022. The MATE Act mandates a new one-time, eight-hour training requirement on the treatment and management of patients with opioid or other substance use disorders for all Drug Enforcement Administration (DEA)-registered practitioners (other than practitioners who are solely veterinarians) who prescribe schedule II, III, IV, or V drugs.
More on Amniotic Fluid Injections
Jul 19, 2023 9:57:00 AM / by J. Kevin West posted in Risk Management, Compliance
We continue to receive questions from podiatry practices regarding the use of and billing for amniotic fluid injections for musculoskeletal purposes. We recently published an article, “Caveat Emptor Vendor: Skin Substitutes & Injectable Amniotic Fluid” that details some real-life examples of the risk providers incur if they fail to do proper due diligence in these situations. In the article below, we continue the conversation around amniotic fluid injections by answering three of the most asked questions so you can make informed decisions at your practice.
Caveat Emptor Vendor: Skin Substitutes & Injectable Amniotic Fluid
Jun 13, 2023 1:52:15 PM / by J. Kevin West posted in Risk Management, Compliance
In the past year, we have seen a dramatic uptick in audits and overpayment claw backs involving two high-dollar products: skin substitutes for wound care and injectable amniotic fluid used for musculoskeletal conditions. While there is no question that these products work, practitioners are often guilty of listening uncritically to sales pitches by vendors who promise high reimbursement and certain payer coverage. Failure to conduct due diligence on these products puts providers at high financial risk because of the substantial cash outlay required to purchase the products, typically upfront.
Coding Changes for 2023
Feb 3, 2023 12:34:52 PM / by PICA Risk Management Specialist posted in Risk Management, Compliance
Background: Big Changes from 2021
The Evaluation and Management (E/M) codes have been based on the 1995 and 1997 E/M Guidelines for what seemed like forever. The E/M codes were based upon three key components: 1) the history, 2) the examination, and 3) medical decision making all performed at the proper levels. On January 1, 2021, everything changed. The changes were specific to Evaluation and Management services that were performed in the office or other outpatient places of service only. Clinicians are now able to use either time or medical decision making to select an E/M code. There is no required level of history or examination for the E/M codes.
Now: Highlights for 2023
On January 1, 2023, the changes that were made to E/M services that were performed in the office or other outpatient places of service were expanded to the other places of service. The E/M codes include a medically appropriate history and/or examination, when performed. The nature and extent of the history and/or physical examination are determined by the treating physician or other qualified health care professional reporting the service. The care team may collect information, and the patient or the patient caregiver may supply information directly (e.g., by electronic health record HERR) portal or questionnaire that is reviewed by the reporting physician or other qualified health care professional. The extent of history and physical examination is not an element in the selection of the level of these E/M codes.
Time is defined as total time spent, including non-face-to-face work done on that day and no longer requires time to be dominated by counseling. It includes time regardless of the location of the physician or other qualified health care professional (e.g., whether on or off the inpatient unit or in or out of the outpatient office). It does not include time spent in the performance of other separately reported service(s).
The definitions of medical decision making (MDM) are the same as the definitions of medical decision making that went into effect for office and other outpatient places of service on January 1, 2021.
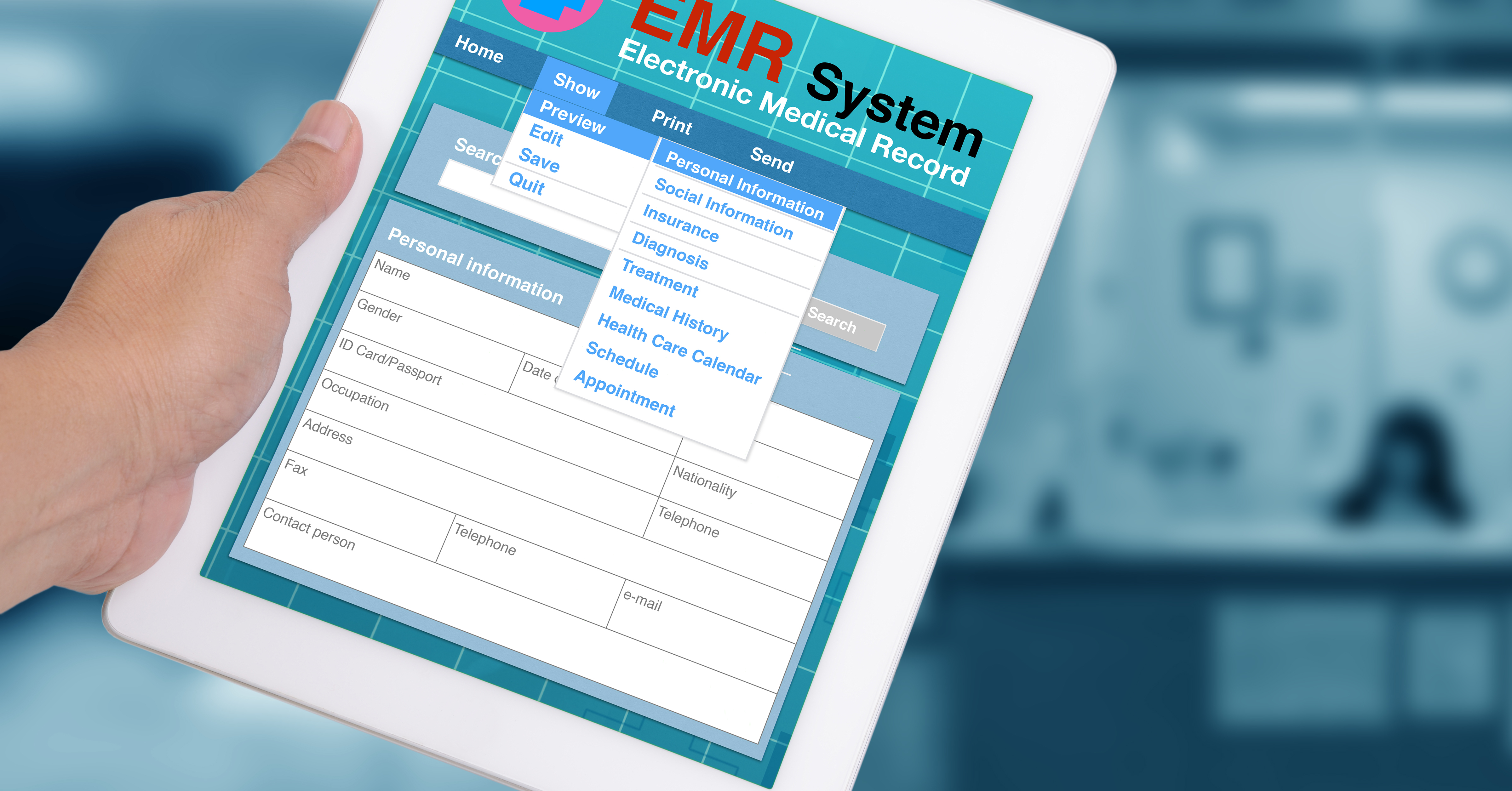
Ask an Expert – Two Common Questions (and Answers!) about EHR/EMR
Aug 15, 2022 1:13:39 PM / by PICA Risk Management Specialist posted in Compliance, Practice Management
We recently received two questions regarding electronic health records (EHR) or electronic medical records (EMR) and thought we’d share the answers in case you’ve asked yourself these questions too.
Here they are: